Women's health: what are the priorities?
Setting health priorities should be a science. A lot rests on it. If you start with the wrong priorities, you not only miss your goals – which means a lot of lives are lost – but you also waste scarce resources in the process; resources that could have been spent preventing even more deaths. Data should speak loudest when determining health priorities – louder than dollars, louder than political power, and louder than legacy investments.
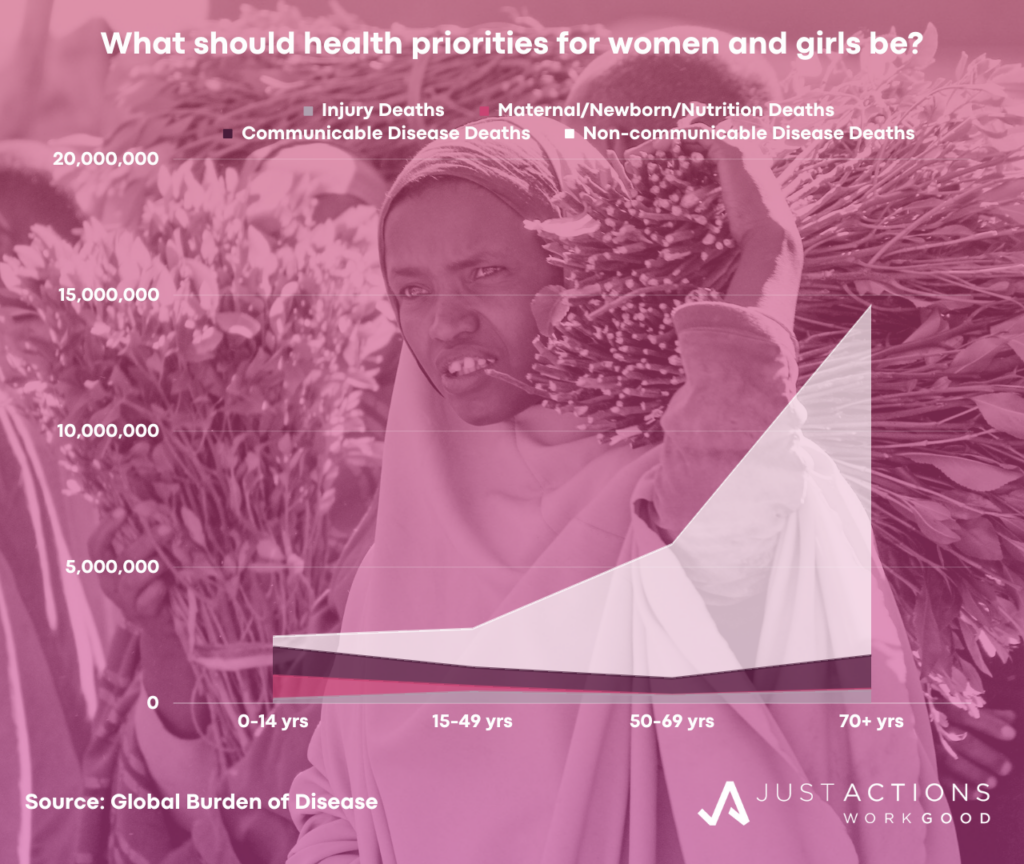
So what does the data tell us when it comes to setting priorities for women’s health? The Global Burden of Disease (GBD), a database that just keeps getting better and better, tells us that 26 million women and girls died in 2019. About 2.6 million are girls under 15, 2.7 million are women 15 to 49 years, 5.8 million are women aged 50 to 69 and 14.6 million are over 70.
What is killing girls and women?
Among girls under 15, it is still the big communicable diseases – pneumonia, malaria, and diarrhea – and several newborn causes, mainly preterm birth, birth trauma, and sepsis. In fact, 40% of all deaths among girls under 15 are now concentrated in the first month of life. But the good news is that these deaths are declining. Deaths among girls have halved since 1990.
Infections remain major drivers of death among women aged 15 to 49 years, principally HIV/AIDs, tuberculosis, pneumonia, and diarrhea. Deaths in pregnancy and childbirth are still killing too many young women, and are the second leading cause of death after HIV/AIDS. Self-harm and road injuries are also leading causes of death among young women.
But it is non-communicable diseases (NCDs) that claim the most lives among women of reproductive age, especially cancers (breast, cervical, and lung), cardiovascular diseases (heart disease, stroke), cirrhosis and chronic kidney disease. Unlike deaths among girls, deaths among women under 50 are not declining. Slightly more women aged 15 to 49 died in 2019 compared to 1990.
Among women aged between 50 and 69, NCDs also dominate, especially heart disease, stroke, diabetes, chronic obstructive pulmonary disease (COPD), and breast cancer. For women over 70, heart disease, stroke and COPD are the leading killers and Alzheimer’s and pneumonia replace breast cancer and diabetes in the top five causes. Deaths are rising sharply for older women driven by aging populations and slow progress in arresting the impact of non-communicable diseases – much of it diet-related.
Priorities matter
So where to prioritize? It matters. There is no doubt that the halving of child deaths since 1990 is largely a result of the sustained focus on child survival over the period and the wider availability of effective technologies especially vaccines, as well as improvements in levels of education, incomes, water, sanitation, and hygiene. In contrast, the major global efforts to control HIV/AIDS among women and to end maternal mortality have a long way to go, and there has been very little attention paid to cardiovascular diseases, cancers, chronic respiratory and kidney diseases, diabetes, and mental health among women.
If we could start over, what would a global priority list for women’s health look like? If we followed the GBD, the list would include a massive new effort to reduce NCD deaths among women under 70, prioritizing heart disease, stroke, COPD, diabetes, and chronic kidney disease. Doubling down on existing efforts to end deaths among women and children from the “big 5” infectious diseases – HIV/AIDS, tuberculosis, pneumonia, diarrhea, and malaria would be on the list. A continued strong focus on ending preventable maternal and newborn deaths and an expansion of the effort to reduce cancer deaths among women under 70, especially breast, cervical, and lung cancers would be vital. And finally, a new global effort to promote mental health, prioritizing reduction in suicide among women, and ramping up the effort to discover new prevention, diagnosis, and treatment technologies for Alzheimer’s disease.
The exact order won’t be the same in every country as disease burdens differ. For example, Africa will need to prioritize the fight against the leading infectious diseases and maternal/newborn deaths, while high-income countries will need to prioritize non-communicable diseases, but not always the same ones. And many middle-income countries in Asia, for example, will need to be active on both.
Technology-enabled self-care
With limited resources to tackle these priorities, many low- and middle-income countries will need to be forensic in their search for the most cost-effective strategies and zero in on those that can directly prevent, or significantly reduce the risks associated with, the leading causes of death. Prevention is not only exponentially better than cure but a whole lot less expensive in most cases. Technologies that give more power to women to “self-care” show particular promise. For example, self-injecting, long-lasting contraceptives will not only prevent unplanned pregnancies, but will reduce preterm births, maternal deaths, and newborn deaths. Home diagnostic tests for leading infections like HIV/AIDS and tuberculosis, as well as diabetes and pre-eclampsia, could increase diagnosis rates triggering faster treatment. Technologies that help women transform their diets could have a huge impact on NCD-related deaths as so many are diet-related.
Technologies from outside the health sector can also deliver a big health impact. Cash-transfers delivered directly to women via mobile money can increase women’s incomes and reduce the risks of infection from transactional sex. Apps to increase literacy rates among adult women have huge potential if we consider that half of the reduction in child deaths in recent decades is the result of increases in education among women of reproductive age, according to an IHME study. Health actors should never forget that 40% of women across sub-Saharan Africa and South Asia remain illiterate, according to UNESCO, and this is arguably the largest barrier to the next wave of women and children’s health improvements.
Empowering women to protect themselves against the leading threats to their health and to diagnose a problem quickly at home is one thing, but technologies that bring treatments closer to home can also save lives. Community health workers who go from home to home in “active case finding” managed by software, “tele-medicine” apps that connect women directly to doctors, and drones that deliver medicines, can all close treatment gaps. Any technologies that improve health while reducing the costs of engaging with the expensive bricks and mortar health system (except for skilled birth and necessary surgeries) are likely to be very good investments.
There should be a name for technologies like these, maybe “technology-enabled self-care.” Prioritizing them may turn out to be the most cost-effective way for countries to transform the health of women and girls, and achieve the sustainable development women’s health goals, especially maternal mortality (3.1), child survival (3.2), communicable diseases (3.3), NCDs and suicide (3.4), and contraception (3.7). Further, the movement towards universal health coverage (3.8) across the globe should embrace the technology-enabled self-care agenda as part of its focus on prevention and primary healthcare.
A final thought. Johan Rokstrom reminds us that countries don’t just have to achieve the new health goals, they have to do it sustainably – in ways that don’t push the planet beyond its boundaries. Simply put, countries have to achieve more in women’s health, with less. By setting the right priorities, and directly giving women the tools they need to protect themselves and their children against those leading threats, technology-enabled self-care may just be one of the best ways to lengthen the life-spans of women and girls and improve the quality of their lives most sustainably.
Updated January 2024