How to invest to prevent early death
In an address titled, “The Future of Aid for Health,” Larry Summers argued that there should be a substantial reallocation of foreign health aid towards global public goods, such as developing medicines and vaccines for diseases of poverty, managing cross-border externalities (e.g., pandemics, antimicrobial resistance), and fostering global health leadership and stewardship, including improving priority-setting processes.
This is a good list, but the most important item is buried at the bottom – priority-setting. Without setting the right priorities for which medicines and vaccines to develop, which externalities to manage, and which leaders to steward, health impact will fall short.
Medical technologies have already contributed significantly to reducing preventable deaths in many countries, but currently no country has achieved all nine of the Sustainable Development Goals (SDGs) for health. While some countries are on track to do so, many will struggle. These are the countries where communicable and/or non-communicable diseases, pregnancy and childbirth, and injuries are still causing tens of thousands, and in some cases millions, of deaths among people under 50 each year.
For these countries, the adoption of technologies that target the leading causes of early death, and the associated risk factors, hold the greatest promise for progress. They are also the areas where foreign health aid and investment can deliver maximum impact.
Priority Populations
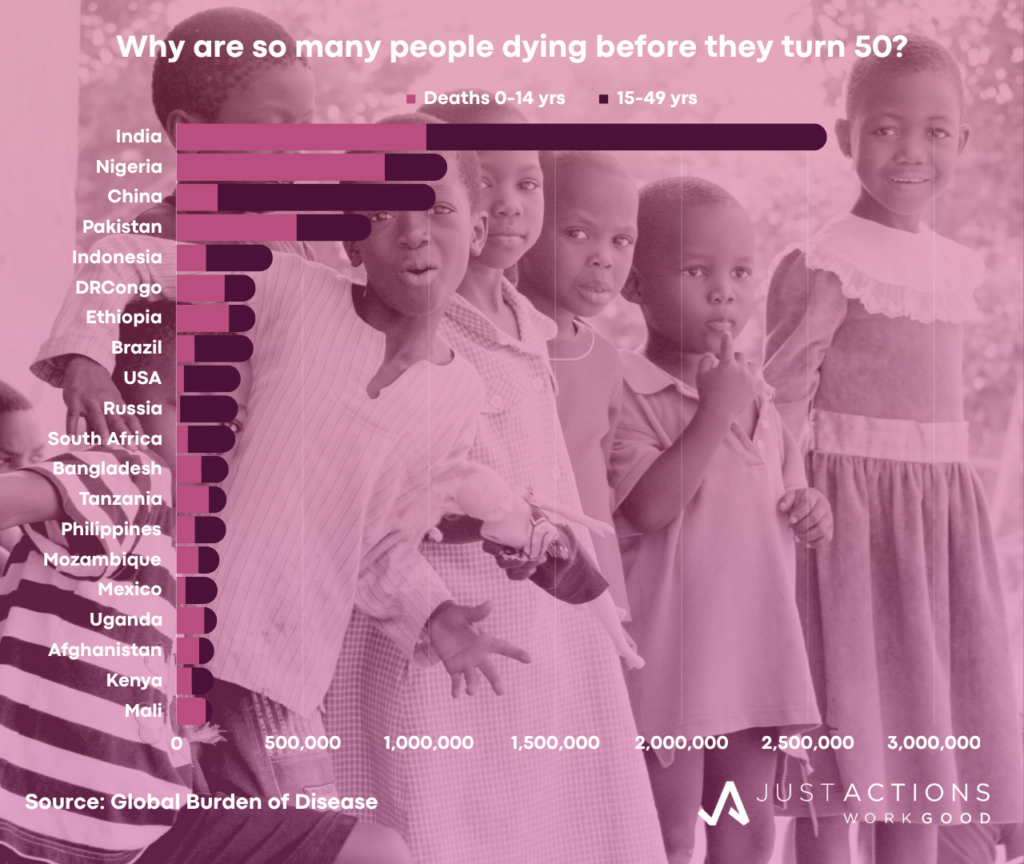
But where are these vulnerable populations, what are the leading causes of early death, and which technologies could save and improve the most lives and dramatically accelerate achievement of the health SDGs? An analysis of Global Burden of Disease (GBD) data reveals 20 countries where more than 140,000 people under 50 died in 2019. India is the clear outlier, with 2.6 million early deaths, but Nigeria and China are also each losing more than 1 million under 50 year olds every year. Pakistan, Indonesia, the Democratic Republic of Congo, Ethiopia, and Brazil are each losing more than 300,000 each year. USA, Russia, South Africa, and Bangladesh are losing between 200,000 and 300,000 people under 50 years. Tanzania, the Philippines, Mozambique, Mexico, Uganda, Afghanistan, Kenya, and Mali are each losing between 140,000 and 200,000.
Although these 20 countries span five continents, including Africa, Asia, North and South America, and Europe, the majority of countries are in Africa (9) and Asia (7) and most are low- and middle-income. In some, early deaths cluster among children (Nigeria, Ethiopia, Tanzania, and Mali), while in others deaths cluster among working-age adults (China, Brazil, USA, Russia, South Africa, Philippines, and Mexico). But some are dealing with heavy burdens of early death among both populations, including India, Pakistan, Indonesia, Democratic Republic of Congo, Bangladesh, Tanzania, Mozambique, Afghanistan, and Kenya.
Early deaths as a percentage of all deaths across the 20 countries range from a low 9% in the USA to a high of 72% in Mali. Most of the countries where more than 50% of deaths occur among people under 50 years are in Sub-Saharan Africa, with the exception of Pakistan and Afghanistan. In contrast, the countries where less than 20% of deaths occur before the age of 50 are in Asia, Europe, and North America.
The rate of progress in reducing early deaths differs markedly across the 20 countries. Between 1990 and 2019, six countries reduced early deaths by more than 50% (Bangladesh, China, Ethiopia, Indonesia, India, and Brazil), while another eight countries achieved reductions below 50% (Pakistan, USA, Russia, Philippines, Tanzania, Mexico, Uganda, and Mozambique). Of concern, early deaths actually increased in six of the countries – Nigeria, the Democratic Republic of Congo, Mali, Afghanistan, Kenya, and South Africa. The countries that recorded the largest decreases in early deaths all achieved major reductions in child deaths over the period.
Priority Causes
Among children, the leading causes of early death are remarkably similar across the 20 countries, but not so for adults. Among children, neonatal causes, principally due to preterm birth, birth trauma, and sepsis, dominate. Congenital birth defects, especially heart defects, are also among the top five causes of child death in all countries. Infectious diseases, especially pneumonia and diarrhea, are major child killers in most countries, followed by malaria in seven countries (Nigeria, Democratic Republic of Congo, Tanzania, Mozambique, Uganda, Kenya, and Mali). HIV/AIDS remains a leading child killer in Russia, South Africa, and Kenya, and congenital syphilis in Brazil and Indonesia. Injuries, especially drowning, choking, and road traffic accidents cause many child deaths in China, USA, and Mexico.
In contrast, among working-age adults, the leading causes of death vary across the 20 countries and between men and women. Among working-age men, injuries are a leading cause of death in all countries, especially road traffic accidents which is among the top five killers of young men in all 20 countries. Self-harm is a major killer in India, China, Brazil, USA, Russia, Bangladesh, South Africa, and Mexico, while interpersonal violence is a problem in Ethiopia, Brazil, Russia, USA, South Africa, Philippines, Tanzania, Uganda, Kenya, Afghanistan, and Mexico. Heart disease, cirrhosis, and/or stroke are leading non-communicable disease killers, while tuberculosis and HIV/AIDS are the leading communicable killers of young men.
Malaria is a leading killer of woiking-age adults in seven of the 20 countries, (Nigeria, Democratic Republic of Congo, Tanzania, Mozambique, Uganda, Kenya, and Mali). Every country except Ethiopia, South Africa, and Tanzania have communicable and non-communicable diseases among the top five causes of early death among young men.
Among working-age women, heart disease is the leading killer in eleven of the 20 countries, followed closely by tuberculosis, breast cancer, and road traffic accidents. Deaths in pregnancy and childbirth remain major killers of young women in nine countries (India, Nigeria, Pakistan, Democratic Republic of Congo, Ethiopia, Bangladesh, Tanzania, Mozambique, and Mali) and HIV/AIDs remains a threat in eight countries, all of them in Africa with the exception of Russia. Other leading non-communicable killers of working-age women include stroke, cirrhosis, diabetes, and chronic kidney disease. Injuries, especially road traffic accidents, self-harm, and interpersonal violence are leading killers of working age women in 13 countries. The six countries where self-harm is a major problem among young women include India, China, USA, Russia, and Bangladesh. Interpersonal violence is a major killer of women in Brazil, South Africa, and Mexico.
Priority Risks
Specific risk factors drive early deaths across the 20 countries. Among children, the top two risk factors across all countries are low birth weight and short gestation (preterm birth) followed by child growth failure (principally child wasting, stunting, and underweight). Unsafe water and air pollution are leading risk factors in most countries, followed by suboptimal breastfeeding, especially in the higher income countries (China, Indonesia, Brazil, USA, Russia, South Africa, and Mexico). Lack of access to hand washing is a major risk for child death in nine countries (Nigeria, Democratic Republic of Congo, Ethiopia, Bangladesh, Tanzania, Uganda, Afghanistan, Kenya, and Mali), and Vitamin A deficiency in five, including India, Indonesia, Brazil, Philippines, and Mexico.
Among men aged 15 to 49, the leading risk factor for early death across the 20 countries is high blood pressure. Only China, Ethiopia, and Mali do not have high blood pressure among the top five risks for early death for this group. Alcohol and smoking are the second and third leading risk factors and no country manages to avoid one or both. High cholesterol and obesity are also major problems in more than half of the 20 countries, only one of them in Africa (India, China, Pakistan, Indonesia, Brazil, USA, Russia, Bangladesh, Egypt, and South Africa). All eight of the countries where unsafe sex is a major risk for early death are in Africa. Of note, diabetes is already a leading risk for early death in two African countries – Democratic Republic of Congo and Mozambique – as well as in Indonesia, Philippines, and Mexico.
High blood pressure is also the leading risk factor for early death among women aged 15 to 49 years across the 20 countries. Only Ethiopia does not have high blood pressure among the top five risks for early death. Obesity is the second leading risk factor but is not yet a major problem in African countries, with the exception of South Africa. In contrast, unsafe sex is a major risk in ten countries, most of them in Africa, but also in Brazil and Mexico. Diabetes is a problem in Pakistan, Democratic Republic of Congo, Indonesia, Bangladesh, Philippines, and Mexico. Air pollution is still a leading risk for death among young women in India, China, Ethiopia, Bangladesh, Mozambique, Uganda, Afghanistan, and Mali due to their higher exposure to household cooking smoke. Diets low in whole grains and fruits and impaired kidney function also feature in the top five risk factors for early death among working-age women.
Priority Investments
Technologies that target the leading causes of early death in the largest populations at greatest risk will have the greatest impact on population health and the achievement of the health SDGs. This means that technologies that can prevent, diagnose, and/or treat the leading causes of early death and/or the leading risk factors among children, working-age women and men in the 20 countries that lose the most young people should be prioritized.
In most countries, this will require investing in the development and uptake of technologies that target four key areas: (1) non-communicable diseases (especially heart disease, stroke, and cirrhosis), (2) communicable diseases (especially pneumonia, tuberculosis, and HIV/AIDs), (3) maternal/neonatal/congenital causes (especially hemorrhage, preterm birth, and congenital heart defects), and (4) injuries (especially road traffic accidents, self-harm, and interpersonal violence).
Technologies that reduce the underlying risk factors associated with early child death would include tools that can reduce the rates of low birth weight/short gestation and child growth failure, and improve access to clean water and air. Among adults the investments that could save the most lives will be able to cost-effectively reduce high blood pressure, alcohol use, and smoking among young men, and high blood pressure, obesity, and unsafe sex among young women.
Child health priorities
For the countries where early deaths are concentrated among children, investments that can target three leading and relatively neglected causes of death are urgently needed – neonatal causes, pneumonia, and nutrition. New tools are needed to prevent preterm birth and congenital birth defects, to diagnose women at risk early in pregnancy, and to treat babies born with complications. In fact, an entire suite of products is needed to retool Neonatal Intensive Care Units (NICUs) in low-resource settings. Technologies that improve the prevention, diagnosis, and treatment of child pneumonia will also save many lives and are the most important infectious disease priority among children. The holy grail is a rapid diagnostic test that can distinguish viral pneumonia from bacterial pneumonia and malaria at the point of care, enabling the more rational use of antibiotics. As malnutrition is driving more than a half of all child deaths, investments that reduce child wasting by improving access to breastmilk (e.g., via human milk banks), and/or other supplements will substantially reduce the risk of child death.
Men’s health priorities
To reduce deaths among working-age men, medical technologies that can prevent, diagnose, and/or treat heart disease, cirrhosis, and stroke will have a major and growing impact, as deaths from non-communicable diseases continue to rise in the 20 countries. Investments that reduces the risks of high blood pressure, high cholesterol, and obesity will further drive reductions in non-communicable disease deaths among young men. However, in many of the 20 countries investments that target the leading communicable killers, especially tuberculosis and HIV/AIDS will remain critical until the spread of these infections has been controlled. In this context, new tools that reduce the risks of unsafe sex, alcohol use, and smoking among young men will have a major impact. Further, investments that specifically target the victims of road traffic accidents, self-harm, and interpersonal violence will prevent many deaths among young men.
Women’s health priorities
Among working-age women, the clear investment priority is reducing deaths from heart disease, followed closely by tuberculosis, breast cancer, and road traffic accidents. Investments that reduce the risk of death in pregnancy and childbirth will remain critical in a subset of African and Asian countries, as will technologies that can prevent the spread of HIV/AIDS. Diagnostic platforms that include the major infectious diseases and chronic conditions that threaten healthy pregnancies are desperately needed and could save many lives. Major increases in the use of long-lasting, self-administered contraceptive devices by a majority of the women in the 20 countries would be transformative not just for women’s health but also for children’s health. Investments that reduce the risks of high blood pressure, obesity, and unsafe sex among young women will prevent the onset of disease and the spread of infections, reducing both communicable and non-communicable disease among young women.
Priority Channels
How these solutions are developed, financed, and ultimately made available in these target populations matters. Innovations that emerge from their country contexts or that are sourced elsewhere and adapted by local institutions, often in partnership with external stakeholders, stand the best chance of success. As private financing for development now dwarfs foreign aid by more than 8 to 1, investments that crowd in private capital to finance both health innovations and access will have the greatest potential for impact. For these investments, success will be measured in the scale of lives saved and sickness averted, and in the way they lay a solid foundation for local pro-health markets to develop.
For those countries where most healthcare is provided by the private sector, investments in companies will yield the highest impact returns. Where private investment dollars – offered as loans, subsidies, guarantees, grants and/or equity – find their way to companies that pursue shared value strategies and/or to local start-up social businesses they have the potential to leave a lasting legacy of better health for future generations. These will be the type of companies that build products to serve one or more of the leading causes of death in one or more of the 20 countries presented in this analysis. Companies with a CEO and management team deeply committed to health impact, and who are as comfortable with public health data as they are with profit and loss statements will have an impact edge. Teams with the ability to craft business strategies that serve both the bottom line and the SDGs, and the skills to work “across the aisles” with governments, universities, and non-profits will represent competitive impact investment opportunities.
For the countries where most healthcare for the vulnerable is provide by government and/or non-profit services, investors will need to find efficient and effective ways to invest directly in government services (e.g. fee for service) and/or to support non-profit services (e.g. grants), being careful not to displace public sector funding for health or to divert talent. Irrespective of the mode of delivery – public or private sector – the most successful investments across all of the 20 countries will be those with a technology or service that passes the price/performance trade-off, either by offering the same solution at a lower cost, by offering a new solution at the same cost, or by offering a new solution that performs better at lower cost (the best investment proposition of all).
Investors that are seeking impact in South Asia should therefore be supporting governments, companies, and or non-profits focused on reducing neonatal deaths, pneumonia, and malnutrition among children, heart disease, road traffic accidents, and tuberculosis among young men, and heart disease, maternal causes, and tuberculosis among young women, with a special focus on India, Pakistan, and/or Bangladesh. Investors seeking impact in Sub-Saharan Africa should support efforts in Nigeria, Ethiopia, Democratic Republic of Congo, Mali, Tanzania, South Africa, and/or Mozambique who are reducing neonatal deaths, malnutrition, and/or infections among children, especially pneumonia, malaria, diarrhea, and/or HIV/AIDS.
With respect to working-age adults, organizations with technologies that can reduce rates of HIV/AIDS, malaria, and tuberculosis as well as the risks of unsafe sex and alcohol use, should be investment priorities. In addition, organizations that aim to reduce deaths in pregnancy and childbirth and iron-deficiency among young women should be on priority lists. In China, Philippines, Viet Nam, and Indonesia, the major investment focus should be on preventing deaths from neonatal causes, pneumonia, and congenital birth defects, as well as reducing the effects of air pollution among children. Among young men, new technologies to reduce deaths from heart disease, stroke, and road traffic accidents, as well as smoking, will have the greatest health impact. In addition, technologies to fight breast cancer, high blood pressure, and obesity will have a major impact on women’s health in the region. It is a similar story in the Middle East where initiatives that target heart disease, road injuries, obesity, cholesterol, and high blood pressure in Egypt and/or Iran will save the most lives.
It is important to note that investors can still make a major impact on health and the SDGs by investing in the large, underserved populations in the USA, Russia, Brazil, and Mexico, where six leading causes of early death dominate – road traffic accidents, violence, self-harm, heart disease, stroke, and cirrhosis. Technologies that target these causes as well as the major risk factors for early death – alcohol and obesity – will deliver major health gains. Investments in governments, companies, and/or non-profits that reach the underserved populations of these four higher income countries do represent high impact health investments in the context of the SDGs.
In summary, the path to global health impact for investors begins with setting the right priorities. By identifying the largest populations at greatest risk of early death and the leading causes and then by investing in the most cost-effective technologies that target these causes in these populations, investors can maximize their impact on health and the SDGs. In countries where the vast majority of health services are delivered by the private sector, investments in companies and social businesses will be essential, while in the countries where governments and/or non-profit organizations dominate health provision, investments the public and non-profit sector actors will offer the most direct path to impact.
Updated January 2024